What Is Testosterone? What Does It Do? How Does It Work?
The first step towards the beginnings of understanding anabolic steroids and how they operate is through the thorough understanding of Testosterone itself. Quite literally, all anabolic steroids are synthetic derivatives of Testosterone, or a modification of a derivative of Testosterone. This is to say that Testosterone’s chemical structure is modified in a variety of different ways, and these modifications are what produce a brand new anabolic steroid – but it is regarded as a Testosterone analogue (or derivative). In this case, Testosterone is what is known as the precursor hormone to the derivative. Other descriptive terms also refer to Testosterone as being the parent hormone, or progenitor hormone of the derivative or analogue hormone. Testosterone is endogenously manufactured by the human body in the Leydig cells of the testes. The term ‘endogenous’ refers to the origin of Testosterone from within the body (referring to production within the human body by the body’s own cells), while the term ‘exogenous’ refers to the origin of a substance from outside of the body (through ingestion, injection, etc.). There exist two other endogenously manufactured hormones within humans that are utilized as progenitor hormones to create anabolic steroid derivatives. These are: Nandrolone and Dihydrotestosterone (DHT).
Testosterone is metabolized into Dihydrotestosterone in the body by way of the 5-alpha reductase (5AR) enzyme (this means that Dihydrotestosterone is a metabolite of Testosterone), and furthermore, Nandrolone is a byproduct of the aromatization (conversion) of Testosterone into Estrogen[1]. With this knowledge, it then stands to reason that Testosterone quite literally is the origin of all anabolic steroids. Without Testosterone, DHT and Nandrolone would not even exist, and therefore without the existence of DHT and Nandrolone, their individual derivatives and analogues would also not exist.
Testosterone itself is the principal male sex hormone. Hormones are defined and classified as chemical messengers of the human body, which means that hormones are what send messages to different cells and tissues in the body to tell those cells and tissues what to do (grow muscle tissue, heal and repair, manufacture important components, perform a specific job, etc.). Without hormones of all different types, all functions within the human body will proceed unregulated and out of control. How much Testosterone the average male produces is dependent on many different factors, which include: individual genetics, age, lifestyle habits, nutritional habits, and activity levels. On average, it has been determined that the median level of Testosterone production among males is between 50 – 70mg weekly. Where any given individual might land within that range is dependent on the aforementioned factors. It is common knowledge that the most prominent effects of the hormone Testosterone appear and are experienced during puberty, which is evidenced by an increase in Testosterone production and secretion, and will typically reach the highest endogenous levels at this point in any given man’s life. This significant increase in Testosterone serves to impart very important physiological changes of the male human body. Testosterone governs many different functions within the body, as is typical of nearly all hormones. The nature of hormones is to govern systemic functions all throughout the body, and Testosterone is no exception to this.
The Importance of Testosterone In the Body and its Functions
As the principal male sex hormone, Testosterone is responsible for governing the development and maintenance of male secondary sex characteristics (deepening of the voice, bodily and facial hair growth, increased sebum secretion on the skin, and development and growth of the male sexual organs which includes spermatogenesis (development of sperm) and increase in libido and sexual function. All of these functions are known as male secondary sex characteristics as well as androgenic (masculinizing) effects and they cannot function or develop properly or efficiently in an environment in which Testosterone levels are inadequate.
Although it is considered an androgenic effect as well, the muscle growth promoting effects have been categorized more independently as an anabolic effect. The word ‘anabolic’ refers to the promotion of tissue growth within the body, and in this case refers to the growth promotion of muscle tissue. This occurs through Testosterone’s ability to signal an increase in the rate of protein synthesis (the rate at which the body can synthesize and create new strands of contractile protein within muscle tissue). Hence this is why males on average naturally are more muscular than females and why males normally carry a heavier lean body weight than females do. Females possess very miniscule amounts of Testosterone, and this can be seen where it has been discovered that the average male endogenously produces approximately 2.5 – 11mg daily of Testosterone[2]. In comparison, females manufacture approximately 0.25mg daily of Testosterone, which is approximately 90% less (or 1/10th) than men. In females, their primary sex hormone is Estrogen, and it too is a steroid hormone, although not an anabolic steroid. By virtue of this distinction, Estrogen exhibits very different effects in the body compared to Testosterone, hence the vast differences between males and females. For example, women naturally possess a ‘softer’ tone and naturally hole more body fat than males do, which is a typical characteristic of Estrogen as it does promote fat retention/storage in various key areas of the body, which is important for female-specific roles (such as pregnancy and fetal development). In addition to this difference, females also exhibit a shorter height, vastly less muscle mass than men, and are far more prone to age-related bone deterioration. This is a direct result of the difference in hormonal dynamics between men and women.
How Testosterone Specifically Works at the Cellular Level
As with all hormones, the systemic and cellular effects of Testosterone are quite intricate, and involve various mechanisms that are both direct as well as indirect in its effects. All anabolic steroids share this property, as essentially, all anabolic steroids are derivatives of Testosterone and therefore possess much of the same properties just as a son shares the same genetic properties passed down from the parent. There are many tissues in which Testosterone exhibits its effects. Of course, the beginnings of the journey in Testosterone’s job involve its transport systemically in the bloodstream as it is pumped throughout the body. Through this avenue of travel and transport, the hormone is free to travel to a variety of target tissues within the body and act as a messenger to tell those cells within those tissues what to do. The specific target tissues of Testosterone include muscle tissue (skeletal muscle), sub-dermal and dermal tissue (beneath the skin and the skin respectively), the scalp, kidneys, bone, the central nervous system, and prostate. What occurs in these tissues is the same general action and activity of all hormones: the hormone binds to a receptor situated either on or within the cell of the particular tissue type, and will initiate a message to the cell to instruct the cell to perform a particular job. In the case of steroid hormones, such as Testosterone and Estrogen, the specific receptors are located inside the cell. Testosterone will specifically bind to androgen receptors there in order to initiate its effects. Only steroid hormones possess the ability to bind to receptors located within cells, as the steroidal nature of Testosterone, Estrogen, Cortisol, or any other type of steroid hormone allows the hormone to be of a fat-soluble nature. This is to say that the hormone will be able to easily pass through 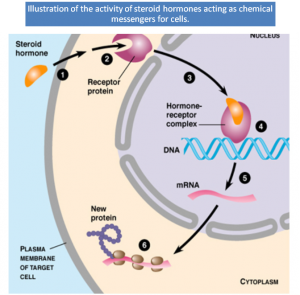 the phospholipid (fat) bilayer of the cellular membrane with ease. Peptide (protein) hormones cannot do this.
the phospholipid (fat) bilayer of the cellular membrane with ease. Peptide (protein) hormones cannot do this.
Other hormone types such as peptide hormones (also known as protein hormones) must bind to receptors located on the outer surface of the cell membrane, as they cannot proceed inside the cell to interact with receptors there. Testosterone can therefore only affect tissues and cells in the body that retain the specific hormone receptor required (the androgen receptor), and therefore will only affect certain tissues and cells in the body. All hormones of all 3 types (steroid hormones, peptide hormones, monoamine hormones) operate in this hormone-receptor interaction, and this is what they all do. Although it is a very vague and non-specific description, the interaction with a hormone binding to a receptor site is described within science and biology as being very much like a lock and key, in which the key is the hormone and the lock is the receptor – both need to fit almost perfectly with one another for a specific action to occur.
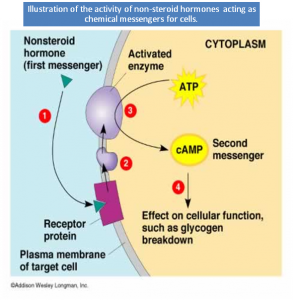 Non-steroid hormones, such as peptide and monoamine hormones operate in the same lock and key manner, but they (as previously mentioned) will bind to and activate receptors located on the outer surface of the cell. The manner by which non-steroid hormones transmit signals through receptors is different from steroid hormones, whereby a peptide or monoamine hormone will bind to the receptor located on the surface of the cell, and this will enable various enzymes and proteins within the cell to act as messengers. These proteins that are then activated as messengers are known as ATP (Adenosine Triphosphate) and cAMP (cyclic AMP), which then travel within the cell to the nucleus of the cell in order to activate gene transcription. Although the general function of non-steroid hormones are the same as steroid hormones, the actual steps and specific action in certain stages is indeed different.
Non-steroid hormones, such as peptide and monoamine hormones operate in the same lock and key manner, but they (as previously mentioned) will bind to and activate receptors located on the outer surface of the cell. The manner by which non-steroid hormones transmit signals through receptors is different from steroid hormones, whereby a peptide or monoamine hormone will bind to the receptor located on the surface of the cell, and this will enable various enzymes and proteins within the cell to act as messengers. These proteins that are then activated as messengers are known as ATP (Adenosine Triphosphate) and cAMP (cyclic AMP), which then travel within the cell to the nucleus of the cell in order to activate gene transcription. Although the general function of non-steroid hormones are the same as steroid hormones, the actual steps and specific action in certain stages is indeed different.
As previously mentioned, Testosterone will enter the target cell(s) by diffusion through the cellular phospholipid bilayer (the layer that encases and encompasses the whole cell), and it will travel through the cytosol (the fluid-filled space inside of the cell) towards the androgen receptor. Once the receptor is located, Testosterone will then bind with the receptor to form what is properly known as the receptor complex. The complex (or ‘receptor complex’) refers to the now bound receptor and hormone together as one. When this occurs, the complex then travels to the nucleus of the cell, which is where it will activate certain DNA sequences. These specific DNA strands/sequences are specific to the intention of Testosterone’s effects on the cell, and they are known as the ‘hormone response element’. For example, in the case of muscle cells, this will activate gene transcription (copying and reading of that specific code of DNA) that will instruct the cell to begin the synthesis and construction of contractile proteins that will ultimately increase muscle strength and muscle size. In layman’s terms, Testosterone is responsible for going into a cell, unlocking the container inside the cell that contains the instructions/blueprints for the cell to do a specific job, and it then tells the cell to do this specific job. In the example given with muscle cells, it informs the muscle cell to begin growth of new muscle tissue. Androgen receptor interaction within other cell types will initiate a different cellular response to the “reading” of these genetic sequences.
Within muscle cells, Testosterone does not only instruct the cell to begin the construction of new muscle cell components (which are the contractile proteins actin and myosin), but also expresses gene transcription of other functions, such as instructing the muscle cell to increase its storage capacity for carbohydrates in the form of glycogen (the useable form of carbohydrates for muscle energy). Following this signaling process, Testosterone will then dissociate (separate) from the receptor, breaking the receptor complex, where it is then free to either linger within the cell before re-engaging in receptor binding, or it may also leave the cell and return to circulation within the bloodstream. It is very important for the reader to understand, however, that this entire process in all of its stages is a slow process and occurs over the course of hours. Studies have demonstrated this time and time again where it has been found that on average, an anabolic steroid hormone requires approximately 4 – 6 hours before the hormone dissociates from the receptor within the cell[3]. These same studies have also demonstrated that new androgen receptors are created after the hormone has broken away from the receptor, which is a very strong indication that androgen receptor sites in fact increase in the presence of androgens, and that the prior theory of many years past that androgen receptors “saturate” as the prime reason for a reduction in progress on an anabolic steroid cycle is quite plainly untrue.
Examples of other areas of the body in which Testosterone and related androgens will exert effects (but in a different end result) is in the kidneys, where Testosterone will, through the same signaling via receptor interaction, signal the cells of the kidneys to begin or increase the manufacture of a hormone known as Erythropoietin (EPO), which is a protein hormone that then travels to bone marrow and signals an increase in red blood cell production[4]. This is what leads to elevated red blood cell and higher hemoglobin levels while on an anabolic steroid cycle. “Hemoglobin levels” and “red blood cell count” are synonymous with one another, as hemoglobin is the protein contained in the center of each red blood cell, which is where oxygen becomes attached to when red blood cells travel to the lungs to pick up oxygen. The red blood cell then travels to various tissues and cells throughout the body to deliver the attached oxygen before returning to the lungs to allow more oxygen to attach to the hemoglobin protein. Therefore, a rise in hemoglobin levels will always correlate with a rise in red blood cell count. The fact is that all anabolic steroids exhibit this effect of erythropoiesis, and although some anabolic steroids will stimulate erythropoiesis to a greater degree than others, they all exhibit this characteristic that is the result of the anabolic steroid’s interaction with androgen receptors in the cells of the kidneys. There is some evidence, however, to suggest that DHT (Dihydrotestosterone) and a few of its derivatives might not exhibit this activity in kidney cells because DHT is very quickly metabolized into non-active hormones by way of the 3-alpha hydroxysteroid dehydrogenase series of enzymes, which are present in very high amounts in the kidneys as well as muscle tissue[5].
This 3-hydroxysteroid dehydrogenase enzyme, which is present in large quantities in muscle tissue (as well as certain other select tissues of the body such as the kidneys) serves to metabolize any DHT that enters muscle tissue into two inactive metabolites: 3-Alpha Androstanediol and 3-Beta Androstanediol. These two hormones, which are metabolites of DHT, are not anabolic at all in muscle tissue. This is therefore the reason as to why DHT is not anabolic in muscle tissue at any amounts, and many chemists and biologists believe that if this enzyme 3-hydroxysteroid dehydrogenase did not exist in muscle tissue, that DHT would actually be a very potent and powerful anabolic steroid. The key benefit in this situation that most DHT derivatives possess is that they contain chemical modifications that allow the hormone to now bypass this limitation whereby the hormone now does not interact with the 3-hydroxysteroid dehydrogenase enzyme and does not become metabolized by it. This allows the DHT analogue to enter muscle tissue (or kidney tissue) and exert its powerful anabolic effects on these cells.
Fat cells are also responsive to androgens such as Testosterone, and although through this they do not impose any dramatic fat loss, they still initiate lipolysis (fat breakdown) in fat cells[6]. It has also been found through this that the interaction of androgens with the androgen receptors in fat cells, the amount of beta-adrenergic receptors is also increased[7]. It is quite evident that Testosterone and related anabolic steroids do play a role in the regulation of body fat levels as evidenced by the fact that when the levels of Testosterone and androgens in general reduce for any reasons, body fat levels will increase[8]. This is very evident in females whom as mentioned earlier possess far lower levels of androgens than do males, but Estrogen also plays an increased role in body fat storage here as well, where Estrogen will increase the promotion and/or retention of body fat in specific areas of the body[9] as well as hypogonadism and andropause patients that will tend to gain increased body fat storage during their years of reduced Testosterone levels. This is one of the reasons that anabolic steroid using athletes and bodybuilders will, through different methods, elect to reduce or control Estrogen levels while on an anabolic steroid cycle. The opposite occurs when androgen levels are increased, where the disposition of body fat to lean mass will become reduced in favor of a body composition that exhibits increased lean mass and decreased fat mass.
Other cells and tissues of the body where Testosterone exerts its effects on androgen receptors includes the sebaceous glands in the skin, hair follicles in the skin, the scalp, the prostate, and certain other areas. The areas such as scalp, skin, and prostate are known as androgen responsive tissues. This is to say that these tissues are responsive specifically to androgens than other tissues, and to greater degrees. Testosterone’s interaction with the cells in these tissues is what brings about the secondary male sex characteristics experienced during puberty. This includes an increase in bodily and facial hair, as well as increased oil secretion of the skin where the sebaceous glands are concerned[10], and thus why acne can become a problem during puberty and during an anabolic steroid cycle in individuals who are sensitive to androgen activity in these tissues. These androgen responsive tissues in particular are designed to be more responsive to the stronger androgen Dihydrotestosterone (DHT), which is what Testosterone is reduced (or converted) into in these tissues. The scalp, skin, and prostate contain high levels of the enzyme 5-alpha reductase (5AR) are present, which is the enzyme that is responsible for the conversion of Testosterone into DHT. DHT binds far more strongly to androgen receptors than Testosterone does, and is therefore a stronger androgen, which is the overall intention in these tissues.
In terms of the scalp and hair loss, which is a common concern among men, it must be understood that the individual must possess the genetic trait for male pattern baldness (MPB) in order to lose hair from increased androgen levels. As mentioned previously, Testosterone and its stronger metabolite DHT can bind to androgen receptors located in the scalp, and through this, trigger male pattern baldness in individuals that possess the genetic trait required for the condition to manifest itself, and can occur in both men as well as women. Those who do not possess the specific gene required for activation will not experience this effect at any dose at all. This is why there are individuals that can utilize the most androgenic anabolic steroids, such as Trenbolone over and over again in cycle after cycle for years, and still end up with a full head of hair in their old age while others less fortunate will use very mildly androgenic compounds and experience hair loss. Testosterone does not, nor do any anabolic steroids cause hair loss – the individual’s hereditary genetics do, and Testosterone will serve to merely speed the process up that has already existed.
Medical Uses of Testosterone and Testosterone Replacement Therapy (TRT)
Testosterone and its associated derivatives and analogues hold a plethora of medical application for the treatment of an almost infinite amount of conditions, debilitations, and diseases. There exist so many applications in fact that they cannot all be covered here, and that an entirely separate article focusing solely on the medical use of Testosterone and anabolic steroids would be required. Testosterone and its analogues have been effectively utilized for the treatment of hypogonadism and andropause, female breast cancer, hereditary angioedema, anemia, muscle wasting diseases such as AIDS/HIV, burn victims, muscular atrophy, male infertility, adolescent growth failure, osteoporosis, female libido problems, Turner and Klinefelter Syndrome, menopause, chronic dysfunctional uterine bleeding (menorrhagia), treatment for endometriosis, and countless other conditions. It is very evident that anabolic steroids are a miracle drug within medicine, and holds the capability to be utilized for the treatment of almost any medical indication as these hormones exhibit systemic effects on the body that can apply to an infinite amount of uses and treatment options. Anabolic steroids and Testosterone has helped to save hundreds of thousands of lives over the previous 70+ years of application and use in medicine, as well as off-label uses.
The primary purpose for Testosterone itself medically, especially in this day and age, is for the purpose of Testosterone replacement therapy (TRT), also known as HRT (Hormone Replacement Therapy), androgen replacement therapy (ART). TRT is normally a therapy administered to individuals who are experiencing lower than normal levels of Testosterone production for a variety of different reasons. The general and proper medical term for this condition is known as hypogonadism, which is a condition in which the testes are manufacturing inadequate Testosterone in individuals and could be due to genetics, physical injury, disease, or any other reason. The specific medical terminology for individuals suffering from age-related decline in proper Testosterone production is known as andropause. The treatment for hypogonadism and andropause are perhaps the most common purpose for the use of Testosterone within medicine in the entire world. It is a simple treatment method that could be easily defined as the supplementation of Testosterone in order to restore Testosterone levels of a male to that of a normal to high range. The majority of patients being treated with Testosterone for this purpose happen to be adult males above the median age of 30, which is a very strong indication that these are mostly andropause patients (those whose Testosterone levels have declined due to aging).
The initial superficial symptoms of low Testosterone are easy to spot signs and symptoms, which include a notable reduction in sexual function and libido (including erectile dysfunction), a notable loss of general daily energy, decline in strength and overall physical performance, depression (to varying degrees), increased bone frailty, decreased motivation, memory loss, and muscle loss[11]. These symptoms occur both in those who experience andropause as well as general hypogonadism. The truth of the matter is that andropause is actually for all intents and purposes, a sub-category of hypogonadism. It is simply a variant of hypogonadism, and could be labeled as age-related hypogonadism. The symptoms listed above are normally very strong indications of lower than normal Testosterone levels, but a general reference range of where Testosterone levels should be are usually given to doctors for ease of reference and determination. This range varies between which medical professional is monitoring blood levels, and which medical organization in which country is setting the standards, but it must be understood that although reference ranges are given, no range is ever set-in-stone, and that doctors should always be allowed to treat their patients according to their unique assessment and judgment of a situation. With this being said, the average ‘normal’ endogenous Testosterone range is considered between 350ng/dl and 850ng/dl. This range of 350 – 850ng/dl, as previously mentioned, can vary (for example, some medical literature suggests a range of 241 – 827ng/dl in some countries/regions/organizations. In general, the 350 – 850ng/dl range is considered the normal range.
Although this 350 – 850ng/dl range is considered the ‘normal’ range, within it there exists a low, mid, and high end within this normal range. For example, if an individual possesses a blood plasma level of 750ng/dl of Testosterone, they are said to be within the high end of the normal range. If an individual possesses a level of 430ng/dl, they are said to be within the low end of normal range. If levels are lower than 350ng/dl, it is regarded as a significant problem (and as mentioned, some medical professionals will lower this minimum level as low as 241ng/dl or lower). As one can see, the threshold for what is considered a ‘normal’ level of Testosterone is actually quite a large one. This is one of the reasons as to why hypogonadism is actually a very much under-diagnosed condition, and many doctors are even still reluctant to prescribe Testosterone for a variety of different reasons (some of which can be regarded as unreasonable). It is important for any individual who suspects they are hypogonadal to seek a doctor who understands, is reasonable, and willing to work with the patient. Most doctors are highly uninformed and uneducated on the issue of hypogonadism and will instead elect (foolishly) to simply avoid touching upon the subject altogether.
It is important after determining the symptoms to then have blood work completed so as to determine with 100% certainty that Testosterone levels might actually be low. No individual can know with absolute certainty whether or not they are hypogonadal until a proper blood test has been done in order to determine Testosterone levels. Because Testosterone replacement therapy will raise Testosterone levels upwards of the normal to high range, it has a high success rate of alleviating all of the aforementioned symptoms. There are various ranges at which different symptoms will become alleviated with TRT. For example, if levels are restored to 350ng/dl or above, the sexual dysfunction and libido is corrected. Testosterone Enanthate administered at 250mg once every 21 days after 6 months demonstrated a 5% increase in bone mineral density[12]. This is a perfect example of how the administration of Testosterone to restore normal physiological levels can help to restore and improve the function of many of the different systems as outlined previously in this article where Testosterone’s effects on the cellular level were explained. This includes increases in red blood cell count, which translates to increased endurance, improvement in energy, well-being, and restoration of muscle mass.
There are various studies that have determined where, on average, Testosterone levels should be in males according to various age groups[13]. These studies have determined the following median blood plasma Testosterone levels according to age:
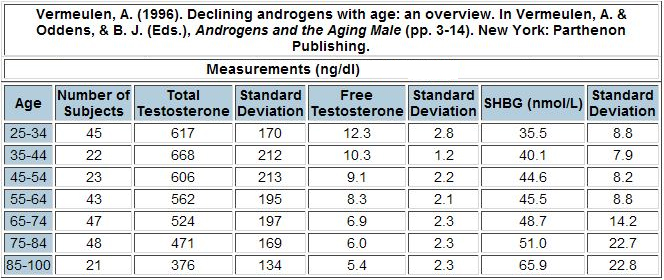
It is important to remember that these numbers are not set in stone, and can indeed be very different depending on the individual in question. It is very important to have a doctor that understands and interprets these functions and results properly. For example, total Testosterone is very different from free Testosterone (free Testosterone is the amount of Testosterone in blood plasma that is unbound by SHBG and free to do its job in the body). SHBG, for those that do not know, is a protein that binds to sex hormones (such as Testosterone, Estrogen, etc.) and renders them inactive, essentially ‘handcuffing’ the hormone, which results in the hormone floating around in the bloodstream doing nothing.
Low Testosterone levels have been associated not only with the symptoms described earlier, but also with a host of other health complications and risks. One such risk in men who possess low Testosterone levels is an increased risk for cardiovascular disease (CVD). Studies have demonstrated that Testosterone used for the purpose of TRT exhibits a positive change in blood lipid (cholesterol) profiles involving a reduction in the ‘bad’ LDL cholesterol, total cholesterol, as well as no changes in the ‘good’ HDL cholesterol[14] [15]. It is normally only once Testosterone levels begin to reach supraphysiological dose ranges that cholesterol alterations begin to change in the negative slightly. In addition to this positive change, the restoration of Testosterone levels to normal-higher ranges has also demonstrated to reduce adipose (fat) tissue in the midsection, lower rates of obesity, and improve the body’s sensitivity to insulin as well as the control of blood glucose[16]. The opposite of these improvements often lead to metabolic complications such as diabetes and obesity, which also further contribute to increased risk of CVD. Testosterone supplementation can also reduce inflammation within the body by increasing levels of the anti-inflammatory cytokine IL-10, and reducing the inflammatory cytokines TNFalpha, IL-1beta, and IL-6[17]. This will assist not only in reducing inflammation systemically, but also protect the arterial walls from the same effects of inflammation.
There are of course some risks and potential side effects associated with TRT. Side effects associated with Testosterone supplementation are the same list of side effects as that of any use of Testosterone, but specifically, elder males seem to encounter a greater degree of potential side effects than younger TRT patients. Because Testosterone is an androgen, it has been found that it might in some individuals induce BPH (Benign Prostatic Hyperplasia) and increase PSA (Prostate Specific Antigen) levels[18] [19]. Prostate hypertrophy is not normally a health or life threatening issue, but can become a discomfort for many, and although Testosterone and related androgens (such as DHT) are not the culprit in prostate cancer, it can play a role in its development provided the environment alongside other contributing hormones is in a perfect position for such a risk. Normal and healthy males that do not exhibit prostate issues prior to TRT do not normally exhibit these problems, and so it is normally advised that men who have (or have in the past had) prostate cancer and/or normally high PSA levels avoid the use of Testosterone[20]. The issue of prostate problems with the use of Testosterone or any anabolic steroids seems to be an issue related to age and of course, genetics. This is evidenced by one study in 2001 investigating supraphysiological (bodybuilding doses, not TRT doses) of Testosterone (600mg weekly for 20 weeks) on 61 healthy males aged 18 – 35 demonstrated no significant impact on prostate-specific antigen (PSA)[21].
Further details concerning the administration and treatment methods of TRT, as well as monitoring blood work results while engaging in TRT will be covered further into this article.
Performance Enhancing and Other Non-Medical Use of Testosterone
To this date, the use of Testosterone for the purpose of performance and physique enhancement is (ironically and hypocritically) an unapproved use by the medical establishment as a whole. This is extremely ironic considering the very first applications of Testosterone were for that of physical and athletic performance enhancement, and the very first officially created analogue of Testosterone, Dianabol (Methandrostenolone), was not designed for any purposes other than for its use as a performance enhancing drug. When Testosterone was first synthesized in the 1930s, the eyes, ears, and complete attention of the whole medical community were on this development and discovery. Almost every individual involved in medicine believed that the use and application of this substance would be unthinkably extensive and far-ranging, and rightly so. These people were correct. The use of Testosterone and anabolic steroids for the purpose of performance and physique enhancement were among its first applied uses, and generally the only reason as to why it is today an unaccepted use by the medical establishment is due to political agenda, political reasons, and political tampering with the medical establishment due to the issue surrounding the “cheating” issue in professional sports.
However, anabolic steroid use for the purpose of performance and physique enhancement remains quite literally its number one use, and far surpasses its use in any other area even in medicine. Anabolic steroids utilized for the purpose of performance enhancement, although it is done illicitly (in the United States), still remains the primary reason for use. Studies have actually in fact demonstrated that the average anabolic steroid user is in fact that of a middle-class heterosexual male of the average median age of approximately 25 – 35 years, and are neither competitive bodybuilders at any level, nor are they professional or amateur athletes at any level either, and these anabolic steroid users are simply utilizing anabolic steroids for purely cosmetic improvement purposes[22]. Many studies have concluded with these results, which then eliminates the rumor and myth that anabolic steroid users for the purpose of performance enhancement consist of only (or mostly) professional athletes or teenage athletes in high schools.
Testosterone is utilized for the purpose of performance and physique enhancement by those attempting to maximize their athletic potential by increasing the levels of hormones (Testosterone), which are already in their bodies. It is quite simple: Testosterone in supraphysiological levels (bodybuilding doses) facilitates a greater and faster increase in muscle strength and size, provided nutrition and training is adjusted to properly favor these effects. It is also utilized by bodybuilders and individuals engaging in fat loss for the purpose of retaining muscle tissue that would otherwise be broken down during periods of dieting (a caloric deficit). Through the assistance that anabolic steroids provide in increases in strength, muscular size, and a decrease in body fat levels are all favored by athletes as well as individuals attempting to improve themselves cosmetically. Testosterone will provide an individual who has reached his or her genetic limits in terms of how much maximum muscle mass can be added, with the ability to surpass this genetic limit. This is often what Testosterone and related anabolic steroids are utilized for, as opposed to the common misconception that they are used as a shortcut.
There exist other non-medical uses of Testosterone that are not as popular, which include its libido enhancing effects. There indeed are individuals for varying reasons that seek to use Testosterone for only one or two of its effects on the body that have nothing to do with its ability to increase muscle mass. However, among off-label (non-medical) uses, the use of Testosterone for performance and physique enhancement is by far the most widespread use. It is even the most widespread use of Testosterone compared to all uses (both medical and non-medical).
Medical References:
[1] Endogenous nandrolone production: studies in granulosa cells from patients with polycystic ovary syndrome (PCOS). W. Schanzer, H. Geyer, A. Gotzmann, U. Mareck (eds.). Sport und Buch Strauss. Koln (2005) 483-486.
[2] Role of androgens in growth and development of the fetus, child, and adolescent. Rosenfield R.L. Adv Pediatr. 19 (1972) 172-213.
[5] Effects of various modes of androgen substitution therapy on erythropoiesis. Jockenhovel F, Vogel E, Reinhardt W, Reinwein D. Eur J Med Res 1997 Jul 28;2(7):293-8.
[6] Testosterone increases lipolysis and the number of beta-adrenoceptors in male rat adipocytes. Xu XF, De Pergola G, Bjorntorp P. Endocrinology 1991 Jan;128(l ):379-82.
[7] The effects of androgens on the regulation of lipolysis in adipose precursor cells. Endocrinol126 (1990) 1229-34.
[8] Visceral fat accumulation in men is positively associated with insulin, glucose, and C-peptide levels, but negatively with Testosterone levels. Seidell JC, Bjorntorp L, Sjostrom L, et al.Metabolism 39 (1990) 897-901.
[9] Effects of Testosterone and estrogens on deltoid and trochanter adipocytes in two cases of transsexualism. Vague J, Meignen J. M. and Negrin J.F. Horm. Metabol. Res. 16 (1984) 380-381.
[10] Effect of Testosterone and anabolic steroids on the size of sebaceous glands in power athletes. Kiraly CL et al. Am J Dermatopathol, 1987 Dec, 9:6, 515-9.
[11] Age related Testosterone level changes and male andropause syndrome. Wu CY, Vu TJ, Chen MJ. Chang Gung Med J. 2000 Jun;23(6):348-53.
[12] Osteoporosis in male hypogonadism: responses to androgen substitution differ among men with primary and secondary hypogonadism. Schubert M, Bullmann C et al. Horm Res. 2003;60(1 ):21-8.
[13] Declining gonadal function in elderly men. Kaufman JM, Vermeulen A. Baillieres Clin Endocrinol Metab. 1997 Jul;11(2):289-309.
[14] Effect of Testosterone replacement therapy on lipids and lipoproteins in hypogonadal and elderly men. Zgliczynski S,Ossowski M et al. Atherosclerosis. 1996 Mar;121 (1 ):35-43.
[15] Testosterone and other anabolic steroids as cardiovascular drugs. Shaprio J, Christiana J et al. Am JTher 1999 May;6(3):167-74.
[16] Androgen deficiency as a predictor of metabolic syndrome in aging men: an opportunity for intervention? Kapoor D, Jones TH. Drugs Aging. 2008;25(5):357-69.
[17] The effect of Testosterone replacement on endogenous inflammatory cytokines and lipid profiles in hypogonadal men. Malkin CJ, Pugh PJ et al. J Clin Endocrinol Metab. 2004 Jul;89(7):3313-8.
[18] Testosterone treatment in hypogonadal men: prostate-specific antigen level and risk of prostate cancer. Guay AT, Perez JB, Fitaihi WA, Vereb M. Endocr Pract. 2000 Mar-Apr;6(2):132-8.
[19] Prostate volume and growth in Testosterone-substituted hypogonadal men are dependent on the CAG repeat polymorphism of the androgen receptor gene: a longitudinal pharmacogenetic study. Zitzmann M, Depenbusch M, Gromoll J, Nieschlag E. J Clin Endocrinol Metab. 2003 May;88(5):204954.
[20] Testosterone deficiency in men: systematic review and standard operating procedures for diagnosis and treatment. Buvat J, Maggi M, Guay A, Torres LO. J Sex Med. 2013 Jan;10(1):245-84. doi: 10.1111/j.1743-6109.2012.02783.x. Epub 2012 Sep 12.





